Abstract
Daratumumab is a human IgG1k monoclonal antibody targeting the CD38 surface antigen on plasma cells with proven efficacy in multiple myeloma. While biology of clonal plasma cells in AL amyloidosis is distinct from myeloma, clonal plasma cells in AL amyloidosis express surface CD38, providing a rationale for using daratumumab. Infusion-related reactions (IR) of 48% were reported in patients who had daratumumab as monotherapy for relapsed multiple myeloma. Therefore, we designed a clinical trial to study tolerability of daratumumab in those with relapsed AL amyloidosis (clinicaltrials.gov identifier: NCT02841033). The primary objective was to determine the safety and tolerability of infusion of daratumumab, with respect to IR. The secondary objectives were to assess hematologic response, clinical response and time to next treatment.
Accrual began in April 2017. Patients with AL amyloidosis after ≥1 prior therapy, and involvement of at least 1 vital organ , eGFR of >20 mL/min, AST/ALT < 3xULN, NT-proBNP ≤8500 pg/mL, LVEF ≥30%, FEV1 ≥50% in patients with COPD or chronic smokers, and ECOG performance status of <3, received daratumumab at 16 mg/kg IV infusion weekly for weeks 1-8, followed by every 2 weeks for weeks 9-24 and every 4 weeks thereafter until progression or unacceptable toxicity, for up to 24 months. The first infusion of daratumumab was given in 1000 mL, the second infusion in 500 mL if no grade 1 or greater reactions occurred, and subsequent doses were administered in 500 mL of saline. All patients received acetaminophen, diphenhydramine, loratadine, famotidine, montelukast and methylprednisolone (100 mg for first 2 infusions and 60 mg thereafter) 30-60 mins prior to infusion. Ondansetron was added after development of grade 1 nausea/vomiting in the first 2 patients. Diphenhydramine, famotidine and methylprednisolone (40 mg) were also administered 2 hrs after start of infusion during the first 2 infusions even if there was no reaction. Methylprednisolone 20 mg (or its equivalent) and montelukast were given 24 and 48 hrs after start of infusion for the first 2 infusions and then it was optional. All patients received prophylaxis with acyclovir.
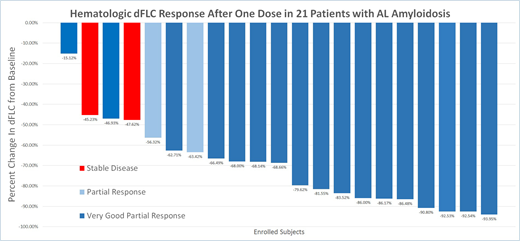
At data cut-off (July 1, 2018) 24 patients were screened and 21 were enrolled. The median age was 65 (range, 42-84), and the median of prior therapies was 2 (range, 1-6): 14 (58.3%) had received SCT, 9 (37.5%) immunomodulatory agents, and 16 (66.6%) proteasome inhibitors. Eleven (52.3%) patients were refractory to prior therapy and the median time from last therapy was 9 months (range, 1-180). The median time from diagnosis to enrollment was 57 months. The median number of organ systems involved was 2 (range, 1-5): 11 (52.3%) had involvement of ≥2 organ systems, 18 (85.7%) had cardiac biomarker stage II or III disease. Median NT-proBNP level was 1346 pg/mL (range, 32-3962) and urine protein excretion was 0.4 g/24 h (range, 0-10.1), while median dFLC was 87.8 mg/L (range, 2.9-328.4). Now, 18 patients are on study and 375 infusions have been completed. The median of infusions received per patient is 19 (range, 3-27). Two patients were removed after developing progression of plasma cell dyscrasia after 2 and 9 cycles and 1 patient was removed by patient choice after 8 cycles. No patient experienced a grade 3-4 IR. Four (19%) patients experienced grade 1 nausea and vomiting during first infusion, which resolved after an antiemetic. The median time of first infusion was 7 hrs and 2nd infusion was 4 hrs 29 mins. Grade 3/4 adverse events were noted in 16 (76%) patients. Respiratory illnesses were experienced by 14 (66.6%), 3 (14%) of these were grade 3 events (Influenza A, Rhino/Enteroviral infection, PCP). Six (28.5%) patients were noted to be iron deficient and required parenteral iron infusion. Hematologic responses were rapid as shown in figure. Hematologic CR and VGPR were achieved by 84.2% (16/19), 85.7% (12/14) and 100% (6/6) patients at 3 months, 6 months and 12 months respectively. Renal response was evident in 37.5% (3/8) and cardiac response was evident in 40% (4/10) at 6 months following initiation of treatment.
Daratumumab infusion is well tolerated in patients with relapsed AL amyloidosis when administered with appropriate supportive care. Infusion-related reactions were minimal and not comparable to reported incidence in myeloma. A rapid hematologic response after 1 dose of daratumumab in patients with AL amyloidosis is seen.
Sloan:Stemline Therapeutics: Consultancy.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal